A recent peer reviewed analysis that appeared on the Centers for Disease Control looked at underlying medical conditions and severe illness (aka comorbidities/preexisting medical conditions) that were found in American adults aged 18 and over who were hospitalized with COVID-19 between March 2020 and March 2021. The study used health records from more than 800 U.S. hospitals for 4,899,447 adults, 540,677 who were patients with COVID-19. Let's look at the analysis
Here is the title page of the research showing the names of the authors:
Let's open this posting with a quote from the introduction which outlines the limits of previous studies:
"As the COVID-19 pandemic continues, a need remains to under- stand indicators for severe illness, defined as admission to an in- tensive care unit (ICU) or stepdown unit, invasive mechanical ventilation (IMV), or death. Several underlying medical conditions among adults, including diabetes, obesity, chronic kidney disease (CKD), hypertension, and immunosuppression, have been reported to be associated with increased risk for severe illness from COVID-19. However, many existing studies are limited in geographic representation, restricted to cases early in the outbreak, or focused on a limited number of preselected conditions and/or severe outcomes. Finally, few studies have shown the effect of the number of underlying medical conditions on the risk for severe COVID-19 illness.
Both the baseline prevalence of a condition and the magnitude of its association with COVID-19 illness help determine the impact of a condition at a population level. This study, based on a large electronic administrative discharge data set, sought to describe the most frequent underlying medical conditions among hospitalized patients with COVID-19 and their associations with severe illness. This information can better inform clinical practice and public health priorities, such as identifying populations for focused prevention efforts and potential vaccine prioritization."
The authors used the Premier Healthcare Database Special COVID-19 Release dated May 11, 2021, a large, US hospital-based, all-payer database. The sample, as noted above, included patients aged 18 years and older who had an inpatient diagnosis of COVID-19 between April 1, 2020 and March 31, 2021. The median age of patients was 66 years, with 48.3 percent being female, 17.5 percent being non-Hispanic Blacks and 17.2 percent being Hispanic or Latino.
The authors examined three indicators of severe COVID-19 illness:
1.) admission to an ICU or step-down unit – 46.2 percent of patients in the study
2.) intermittent mandatory ventilation (which is defined as a type of control mode ventilation in which the patient breathe spontaneously while the ventilator delivers a prescribed tidal volume at specified intervals and allows the patient to breathe spontaneously between cycles. The ventilator rate is set to maintain the patient's PaCO2 at desired levels and is reduced gradually to zero as the patient's condition improves) – 14.2 percent of patients in the study
3.) death – 14.8 percent of patients in the study
The authors considered each patient's specific underlying medical conditions and the number of these conditions. The They used a multistep approach to identify the underlying medical conditions and selected the most frequent conditions (of which there were 18) which had a prevalence of ten percent or more in the sample.
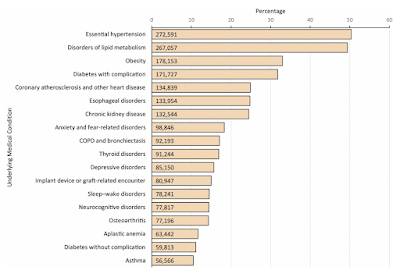
Let's look at what the authors found. Here is a bar graph showing the prevalence of the most frequent underlying medical conditions in the sample:
The top five preexisting medical conditions are as follows:
1.) hypertension (high blood pressure)
2.) disorders of lipid metabolism (which most of us would associate with high cholesterol) – 49.4 percent of patients
3.) Obesity – 33 percent of patients
4.) Diabetes with complications – 31.8 percent of patients
5.) coronary atherosclerosis and other heart disease – 24.9 percent of patients
To put these numbers into perspective, the percentage of the United States adult population known to have two or more medical conditions ranges from 38 percent to 64 percent, depending on the persons' state of residence.
The authors also calculated the relative risk of death in relation to the associated medical condition:
1.) 30 percent higher for patients with obesity
2.) 28 percent higher for patients with anxiety and fear-related disorders
3.) 26 percent higher with diabetes with complications
4.) 18 percent higher with neurocognitive disorders including dementia and Alzheimgers
5.) 18 percent higher with chronic obstructive pulmonary disease and bronchiectasis
6.) 14 percent higher with coronary atherosclerosis and other heart disease
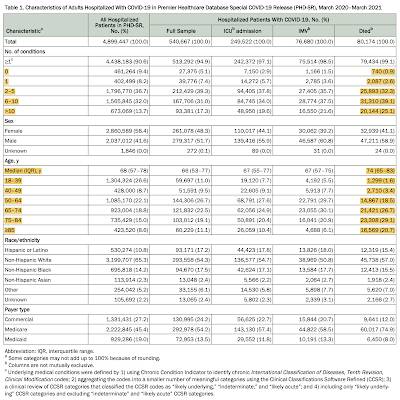
Compared to patients with no documented underlying medical conditions, patients' risk of death increased based on the number of underlying medical conditions that they had as follows:
1.) one condition – 1.53 times greater
2.) two to five conditions – 2.55 times greater
3.) six to ten conditions – 3.29 times greater
4.) more than ten conditions – 3.82 times greater
Most importantly, the authors found the following for patients that died (median age of 74 years):
1.) only 0.9 percent had zero underlying medical conditions
2.) 2.86 percent had one underlying medical condition
3.) 32.3 percent had two to five underlying medical conditions
4.) 39.1 percent had six to ten underlying medical conditions
5.) 25.1 percent had more than ten underlying medical conditions
Here is a table showing the key data, noting that I have highlighted the relationship between the number of conditions and age as it relates to death among those hospitalized with COVID-19:
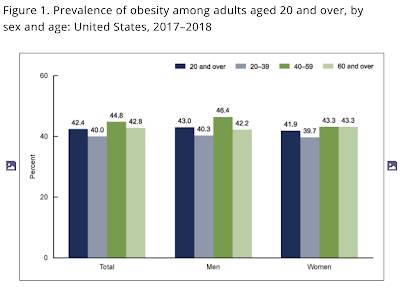
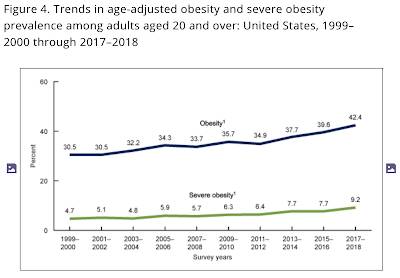
As you can see, in the United States, those who were hospitalized for COVID-19 were more likely to die if they had a high number of pre-existing medical conditions. Interestingly, the three factors that were most common among those who were hospitalized for COVID-19 are all related to obesity (including obesity itself) and, given its prevalence among the adult American population, this factor may go a long way to explaining the high number of deaths associated with COVID-19 in the United States as shown on these two graphs from the CDC:
You can publish this article on your website as long as you provide a link back to this page.

Be the first to comment